Health & Wellness Curriculum | A Whole Person Care Status Report
/Telecare has a long-range plan for expanding and deepening its Whole Person Care (WPC) efforts. We began by examining
co-occurring conditions—educating providers and ensuring that Telecare’s Co-Occurring Education Group is available in all our programs. Right now, we are laying the foundation for future efforts by focusing on health literacy.
We recognize that behavioral health providers need support as they work with clients to address their physical and substance use issues. In May 2016, Telecare introduced Phase 2 of our Whole Person Care initiative: health literacy. The Health & Wellness Curriculum consists of eight online modules on topics such as Diabetes, Cholesterol, Blood Pressure, Managing Our Stress Response, Tobacco Use, and more. Each module is accompanied by visually engaging and easy-to-follow handouts that staff can use to engage clients in conversation about these health concerns.
Though we’re still early in our company-wide implementation, the feedback so far is promising. Here is an update on our progress, as of April 2017. Below, you’ll find:
Where We’re Going: Implementation Timeline & Status Update
What We’re Seeing: Early Discoveries From the Field
More Info: Whole Person Care Goals
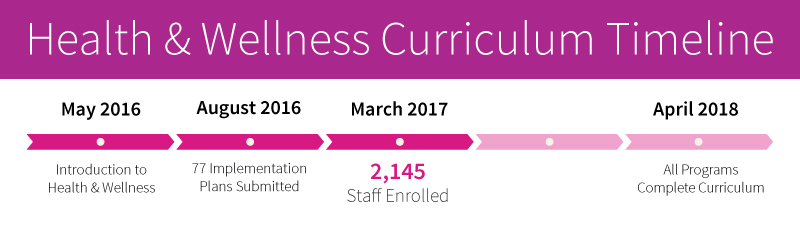
Implementation Timeline & Status Update
Right now, we are working on Phase 2: health literacy. Telecare’s programs have the flexibility to implement the health and wellness literacy curriculum at their own pace, but all programs must complete the curriculum by April 2018. Here is a snapshot of our progress over the last year.
Early Discoveries from the Field
We spoke to staff at three Telecare programs that are moving quickly to fully implement the Health & Wellness Curriculum, a 16-hour, online training program that provides staff with basic knowledge about the chronic health conditions that our clients most commonly face. Here’s what staff have told us about the curriculum’s impact so far.
We're Increasing Linkages to Primary Care
Erich Stevens, Registered Nurse
San Diego Gateway to Recovery
Early discoveries:
More conversations happening
More linkage to primary care
More physical health therapy
How the curriculum has helped:
"I think the modules and quick reference tools for use in the field have been extremely helpful to case managers and other non-nursing staff in better understanding these health issues and how to assist clients with them, which has typically been up to the nursing staff alone."
Why do it:
“It gives us more ways to help clients reach a higher level of wellness.”
Clients Are Taking More Initiative in Setting Doctor Appointments
Tienna Jackson, Team Lead
Gateway to Recovery
Early discoveries:
Clients willing to make primary care appointments
More physical health therapy
Increase in health conversations
How the curriculum has helped:
“The worksheets that were available with each module were given to members to help support them in whatever their hopes and dreams are in regards to their health and wellness.”
Why do it:
"It reinforces to our staff the importance of addressing both the medical and mental health aspects of recovery with our members, and really, it has been working. Our clinicians and nurses are coming back with stories of how they tell people the importance of seeing a doctor, and members are open to making appointments with their primary care provider on the spot."
We’re About to Help Clients Better Understand How Physical Health & Mental Health are Connected
Rocio Perez, Clinician, Los Angeles Older Adults
Early discoveries:
Handouts help show clients how mental and physical health are connected
Increased efforts towards self-care
How the curriculum has helped:
“The Health & Wellness Curriculum has been especially helpful partnered with psychoeducation. One example is around diabetes. Many of our members are diabetic, and they don’t know what it is to be diabetic, or how it affects your mental health. Having the handouts have made it easier to talk with clients about the different ways to address living and dealing with physical ailments.”
Why do it:
“For me, being mentally OK and being physically OK go together, which is how we have implemented it in our office, and I see it working.”