NatCon2018 Presentation: An Organization’s Incremental Journey Toward Whole Person Care: Practice Improvement in Real Life
/In 2010, Telecare began a journey to Whole Person Care, bringing greater focus on healthcare and substance use services into our behavioral health programs.
With limited resources to draw upon, we needed to be cost-conscious and choose approaches that offered the greatest impact and leverage.
In April 2018, we shared our journey and lessons learned in an iPoster session at NatCon18.
View a PDF of the Presentation
Workforce Development
As we began to develop our Whole Person Care plan, we found that we needed to address the training challenges of our geographically diverse and multidisciplinary workforce. Telecare has nearly 3,500 staff spread over seven states and a very diverse workforce of behavioral health providers and nursing staff. The entire range of our staff needed to understand the importance of whole health as well as have knowledge of co-occurring substance use and chronic health conditions, and be able to use tools to engage clients and enhance motivation through stage-matched conversations. To address this, we developed an 18-hour Whole Person Care eLearning program that covers stages of change, substance use and addiction education, as well as significant facts on chronic health conditions, culminating in an earned certificate.
Clinical Practice Improvement
We needed to update and enhance our current clinical practices to include whole health education and lifestyle modifications, as well as explore clinical models for coordinated care that improve outcomes and reduce costs for customers.
Our Co-Occurring Education Groups (COEG) were developed to reach people in pre-contemplation and contemplation stages of change around substance use. We also created “Smart Sets”: Decision trees that enforce key elements of health integration and identify touchpoints for motivational enhancement. We also partnered with customers to build new coordinated care clinical models that improve outcomes while reducing costs. We tested and refined new processes and then disseminate them broadly to the rest of our programs. Finally, we identified several interdependent evidence-based practices and developed a clinical framework to bring them to staff, matching the critical skills to staff roles and client acuity levels.
Client Education
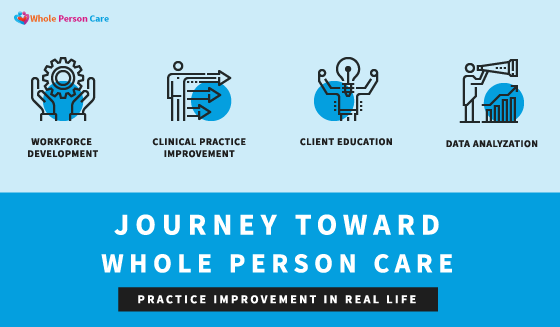
The people we serve often do not understand their high-risk physical health conditions, nor do they have fact-based information on the effects of substance use on their health. To assist our mental health providers in regularly educating and engaging clients in conversations around their health conditions, Telecare created easy-to-read, visually-engaging handouts that present a range of whole health topics, including blood pressure, body weight, diabetes, and asthma. The handouts provide education on facts and effects about each condition and offer suggestions for how to manage or prevent the condition. They also inform and empower clients by suggesting lifestyle changes that can directly improve their health and wellness.
Staff have reported increased confidence initiating conversations by using these handouts, and clients report that they are learning information about their conditions for the first time. We have translated these handouts into six threshold languages to increase accessibility. Our workforce benefits from the handouts as well: staff report that they are using the handouts to learn about and manage their own chronic health conditions.
Initial Outcomes
Telecare’s Partners in Wellness, the first mental health Pay for Success program in the nation that incorporates our Whole Health tools, is surpassing its success targets, with excess savings of more than $500,000 in the first year. Another program, Inland Empire Health Plan (IEHP), a population management program for high utilizers, has shown statistically significant reductions in psych inpatient, psych ER, medical ER, and IOP utilization, as well as increased contacts with their primary care physicians. (See poster for more details.)
Lessons Learned
We have learned that the following practices greatly enhance our ability to integrate Whole Person Health into our programs:
Educating our senior leadership team first. Senior leaders must fully understand and be "on board" with new practices and clinical models before roll-out to the company at large.
Engaging all staff to see health equity as a social justice issue, which helps us advocate for the people we serve.
Communicating clearly and consistently to ensure comprehension and buy-in from staff.
Adapting plans as funding appears and disappears; being nimble allows us to keep up with changes in the healthcare environment.
And finally, remembering that small steps matter! Sustaining momentum is important when introducing and learning from new models of care.
More Information
Kent Eller, MD, Telecare Chief Medical Officer
Shannon Mong, Telecare Director, Innovation Initiatives
Faith Richie, Telecare SVP of Development
Telecare Whole Person Care Brochures and Information
Reaching the Unreachable (Substance Use)
Care Coordination Case Study (IEHP)
Health & Wellness Curriculum (Physical Health)
The Morning Huddle (Data-driven Care)